INTRODUCTION
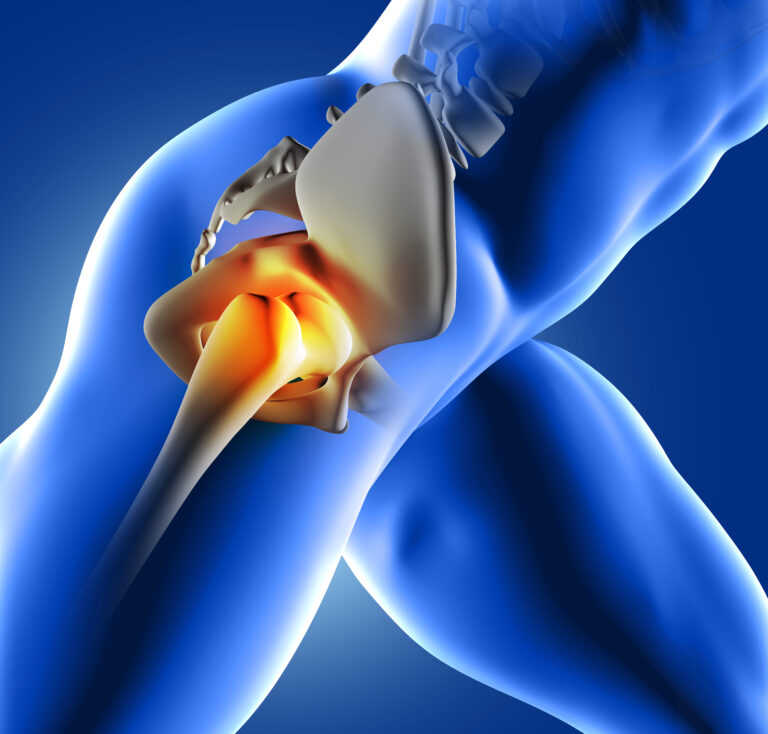
Femoroacetabular Impingement (FAI) is described, as a pathomechanical process (1,2) believed to be the result of abnormal contact between the proximal femur and the acetabulum (3,4). The deformities that result from FAI have been linked with early onset osteoarthritis, primarily in active adults due to the repetitive loading of the cartilage within the hip joint (3,5) Research has shown that the prevalence of FAI within the athletic population is much greater than that of the sedentary population or control groups (6,7), therefore supporting the link between repetitive loading through an abnormal cartilage and early onset osteoarthritis. However although this link is supported, an important factor to consider is whether or not the intense training carried out by athletes is the cause of abnormal changes within the hip joint, or merely an aggravating factor.
Several mechanobiological and biomechanical studies have been conducted in order to determine the development of hip joint deformities in relation to FAI (5) with some research arguing that genetics have an involvement (8).
FAI is a generic term for impingement symptoms resulting from abnormal changes within the hip joint, but these changes are further divided into 3 types of FAI. Cam-type occurs when there is an abnormal defect of the femoral head, resulting in a loss of sphericity (2). Pincer-type occurs when an abnormal defect of the acetabulum is present, and mixed type is a result of Cam and Pincer being present simultaneously (5). Previous research has shown that Cam lesions are more prevalent in active young men, while Pincer lesions are often found more in active middle-aged women
(9). However, there is also research to suggest that mixed-type lesions are more prevalent than Cam-type or Pincer-type occurring in isolation (9), with some finding mixed-type to occur in more than 90% of cases (2). This finding has been disputed by research that analysed the morphology of 60 acetabula through the use of CT scans (10). The results of this study are open for interpretation as it suggests that cam-type lesions typically have a shallower acetabulum than normal hips, consequently meaning they are shallower than pincer-hips. This therefore gives the impression that it is not possible for cam-type and pincer-type lesions to occur in conjunction with each other, due to them being different patho-anatomic entities. However research into the prevalence of the different FAI types and the populations they affect is lacking and more needs to be carried out in order for efficient comparisons to be made and for a more definitive conclusion to be reached as to the causes of FAI in varying populations.
Research into FAI has rapidly developed due to an ever-growing clinical interest, prompted by an increased prevalence. The number of publications on FAI between 1999 and 2007 was significantly higher than previous years (1), with the focus varying from aetiology to treatment, but with a vast majority being review articles. Biomechanical implications as a result of long-term FAI has been widely researched, however there appears to be considerably less research into possible biomechanical alterations as a causative factor of FAI. The majority of the biomechanical research is primarily focused on gait or stair climbing in people successfully diagnosed with FAI through radiographic imaging (11-14). This article intends to discuss the different perspectives on the relationship between biomechanics and FAI, with the key focus being how certain altered biomechanics may act as a contributing factor to the onset of FAI.
Aetiology:
The purpose of the hip joint is to enable weight bearing during movement; this is often affected by the changes within the joint caused by FAI, primarily during extremes of movement (9). Patients with possible FAI typically present with signs of hip, groin, and back pain, which worsens with movements that involve excessive hip flexion, adduction, and internal rotation (15,16). These are movements required during everyday activities such as prolonged sitting or walking, deep squats, and stair climbing. The primary cause of FAI has been suggested as being due to the contact between an abnormal femoral head and neck, with the acetabulum. This repetitive contact causes damage to the acetabular cartilage, which results in labral tears that present as hip pain (9). There is some evidence to suggest that childhood hip diseases such as Perthes disease, slipped capital femoral epiphysis (SCFE), and hip dysplasia are arguably precursors to FAI in adulthood (17). Similarly, some research has shown that stresses placed on the hip joint through repetitive sports or trauma, as well as some potential genetic links can aggravate an already developed FAI (1). However no definitive aetiology of FAI has yet been identified (1), thus there is a clear a window of opportunity for further research into altered biomechanics as a potential aetiological precursor into the development of FAI.
The most significant risk factor for the development of FAI is as previously mentioned, childhood hip pathologies (17). However, other biomechanical abnormalities may also have detrimental effects on the hip joint. For example, a study focusing on the reliability of Beighton score when assessing hypermobility in FAI patients found a significantly high prevalence of hypermobility within the FAI population assessed (32). It could therefore lead to the development of future studies researching in depth the link between hypermobility and FAI. Similarly, although there is limited research, it is plausible to suggest that knee and foot abnormalities can also contribute to the development of FAI, as we know that biomechanically they all work in conjunction with each other, thus if one is misaligned it can have significant effects elsewhere in the kinetic chain. However, due to the lack of research it can only be taken as a hypothetical relationship until further research is carried out, giving definitive evidence.
FAI & Biomechanics:
Several studies into the relationship between FAI and biomechanics have been undertaken, however the primary focus is more often than not how FAI affects biomechanics rather than biomechanics as a causative factor. Studies have shown that FAI has a significant effect on biomechanics during various stages of gait. One study in particular suggests that there is a noticeable increase in ankle dorsiflexion and hip flexion as a result of increased acetabular cartilage abnormalities leading to a reduction in hip function (12). Although this study provides a good insight into how FAI affects hip and ankle biomechanics, it would have been beneficial to also show spinal movement throughout gait as alterations higher in the kinetic chain may also lead to increased loading at the hip joint. The study also uses a six minute walking test, where the speed is self chosen, thus it is possible to argue that the results are not completely viable as the speed may vary drastically between participants, causing varying amounts of stress on the hip joints of each participant. This study does make it clear that ankle biomechanics may be a compensatory mechanism to allow for optimal achievement of every day activities such as walking. However it also suggests that the relationship between altered ankle biomechanics and FAI is not completely known, as there is a possibility for it to be causative rather than compensatory (12). Due to the uncertainty of biomechanics as a causative factor or simply an aggravating factor, there is a definite opportunity for further similar research to be carried out.
Further research has suggested that FAI may be associated with alterations in hindfoot mechanics (13). Through a three-dimensional gait analysis it was concluded that in patients presenting with cam-type FAI there is repetitive excessive inversion of the hindfoot during the heel strike phase of gait, followed by a reduction in maximum eversion during the stance phase (13). Although this study does not determine whether FAI is a cause of altered biomechanics, or altered biomechanics are a precursor of FAI, it provides an adequate foundation for future studies to investigate the relationship between FAI and hindfoot biomechanics. This study was conducted solely on men presenting with cam-type FAI symptoms, thus it provides a basis for similar studies to be conducted focusing solely on women with various FAI types, which in turn may lead to sufficient comparisons to be made due to minimal differences in study design. Reproducing this study on women would also allow for conclusions to be drawn in relation to the varying types of FAI and the populations they affect. Similarly to other research investigating the effects of FAI on gait, it can be argued that simple walking is not challenging enough to effectively show the complete effects of FAI on biomechanics, as extremes of motion are not tested. It may therefore be worthwhile repeating this study in a running or stair climbing motion to further identify how gait is affected by cam-type FAI in males, or vice versa.
Another study into the effects of FAI on gait suggests that there are no impairments of hip kinetics in patients shown to have positive FAI through radiographic screening (14). This study provides a very small sample size (n=15) which suggests that the results may not be a true representation of the relationship between FAI and gait. The assumption may once again be made from this study that perhaps walking is not a challenging enough task to elicit the compensatory movements often shown by patients with FAI. If this is the case then further research must be done that allows the hip joint to enter extremes of range, ideally through measuring running kinematics as this also elicits extra force through the joint. Research has suggested that individuals with FAI may activate alternate muscle groups as a protective mechanism for the hip as it is forced into end of range movements (18). This suggests that future research would need to focus on a combination of measuring biomechanics along with possible muscle activation throughout various movements. Ideally future studies will also carry out testing in more than one plane of motion to allow for rotation of the femur or tibia to be taken into consideration.
One of the most recent studies focuses on lower limb biomechanics during stair climbing, which is a necessary development from previous studies focusing solely on gait. The research suggests that while ascending stairs subjects with FAI present with increased peak trunk flexion and external hip flexion moments, and furthermore they show a decrease in peak external knee flexion (11). This study also took into consideration self-reported hip pain and function on the day of testing by using the Modified Harris Hip Score (MHHS), which has arguably been shown to be quite a valid and reliable method (19). Taking into consideration pain levels while testing is important as it provides a potential explanation for compensatory movements. There is a possibility that compensations are made due to pain rather than the bony alterations within the joint. This study provides a more challenging method of testing, arguably making the results more usable when deciding how to effectively treat the symptoms of FAI. Unfortunately, this study has one key limitation in that their control group was based on the absence of back and hip pain rather than radiographic findings. This may affect the results of the study as previous research has shown that asymptomatic FAI occurs in approximately 33% of positive radiographic findings (20). Similarly, due to the variation in pain levels between the participants, there may have been differences in stair climbing performance, which may have caused inconsistencies with the results. However, due to the study design it remains a key development within FAI research, which will enable similar studies to be carried out in the future, that provide more in conclusive results.
Investigations & Diagnosis
Clinical investigations into FAI rely heavily on the subjective history of the patient, in conjunction with a few key impingement tests. There is typically an insidious onset of pain, usually in the groin region that is associated with activity (9). Patients also present with an inability to perform movements requiring extreme ranges of hip flexion, and experience painful clicking and locking within the hip (9). The clinical impingement test is commonly used to diagnose FAI; it is deemed positive if it elicits the symptoms of FAI. The impingement test forces the hip into extreme ranges of flexion, adduction and internal rotation (21). The Flexion, Abduction, External Rotation (FABER) provocation test is another clinical test used to aid in the diagnosis of FAI. It is once again deemed positive if it reproduces the symptoms usually felt by the patient (22).
Bony abnormalities within the hip joint can be successfully depicted using various types of radiographs (23). Computerised Tomography (CT) scans have high resolution for detecting FAI, however due to the high does of radiation it should be used with caution (24). Pritchard and O’Donnell developed the concept of CT scanning in the position of discomfort, as this enables symptomatic cam-type deformities to be successfully identified (9). The most commonly used form of radiographic diagnosis is a high resolution MR arthrography (MRA), as it is the preferred method for suspected labral pathologies (9). Both MRA and CT scans are capable of detecting the alpha angle, which is the angle connecting the centre of the femoral head to the point of commencement of femoral head flattening (9). It has previously been found that the average alpha angle in a cam deformity is 65-70° while a normal femur is suggested to be 42-47° (25). It has been found that CT scans in the position of discomfort are the most effective in detecting bony hip normalities, and are therefore most relied upon whilst diagnosing FAI (9). However, as previously mentioned there are several cases of FAI that remain un-symptomatic, therefore regardless of radiographic or clinical findings, it is important to treat based on what the patient presents with.
Management
FAI typically requires surgical intervention, and it is believed that clinically and radiographically diagnosed cases of FAI should be corrected via surgery before the bony abnormalities become irreversible (1). Surgery is predominantly aimed at removing the mechanical obstruction between the femur and the acetabulum (26), however it is also important that any labral tears within the hip joint are also addressed (9). There are currently two surgeries that are used; open surgery and arthroscopy. Open surgical procedures are carried out by dislocating the hip anteriorly, to allow a 360° view. The bony abnormality that is causing the impingement can therefore be clearly visualised and removed to re-establish the concavity of the femoral neck junction (9). Open surgery runs the risk of avascular necrosis or fracture of the femoral head and neck (27). Arthroscopy is increasingly being used as a form of intervention for FAI (9), however research has suggested that it compromises the complete examination of the femoral head and neck (28). Arthroscopic techniques are predominantly used for debridement of labral tears, repair of a torn labrum, drilling or micro-fracture of acetabular lesions, and capsular excision (9). However several studies have shown that treating labral abnormalities through techniques such as those previously mentioned, without treating the true FAI causes is a major reason for treatment failure (29,30).
Although conservative treatment in the form of physiotherapy and anti-inflammatory therapy are the initial interventions for FAI, there is minimal evidence to suggest they have any benefits (1). Predominately modification of activity is done to ensure minimal excessive hip movement; this is then followed by non-steroidal anti-inflammatories to aid with symptom relief (9). Research has shown that conservative treatment can have some benefits in the form of a 4-phase treatment. Firstly activity modification and anti-inflammatories, followed by 2-3 weeks of physiotherapy in the form of stretching to improve external rotation and abduction in flexion and extension. An assessment is then done to find the normal hip range of motion for each patient once the acute pain has subsided. Finally, each patient is advised how to modify daily living activities that may be predisposing factors to FAI, this includes avoiding cycling and where unavoidable, adjusting the seat height to avoid extreme hip flexion. Similarly patients were instructed to avoid sitting for long periods of time with hips flexed and spine straight, to lean back every so often to enable the hips to be stretched. The results of this study show 27/37 participants having significantly improved symptoms following a 2-year follow up, with 6 having minimal improvements and 4 having required surgery (31). Therefore although it is not necessarily suitable for all cases of FAI, there can be some benefits from conservative treatment. However this study does not include patients with previous hip pathologies such as Perthe’s disease, which has been shown to be a possible pre-cursor to the development of FAI. It would therefore be beneficial for further studies to be carried out that potentially include a variety of previous hip-pathologies.
Discussion
The increase in prevalence of FAI within a variety of populations has without a doubt prompted a large amount of new research to be carried out. However, as previously mentioned throughout this article there is a significant lack of research that focuses on the direct relationship between FAI and biomechanics. Furthermore, biomechanical abnormalities have clearly been shown to have connections with FAI, though whether these are contributing factors to its development, or merely aggravating factors of an underlying hip pathology is yet to be determined. Either way, it is important to address biomechanics when conservatively managing FAI, as whether it is a contributing factor, or an aggravation, correcting biomechanics should allow for some relief. Again, this is an area that requires further research before it is used within the management of FAI.
Research to date has provided us with a solid foundation on which we can build possible theories as to the aetiology of FAI (5). The majority of the research published has shown some changes in lower limb biomechanics in participants with FAI (11-14). However, the question again arises as to whether these changes are compensatory due to the hip pathology, or causative as a result of altered biomechanics combined with a high intensity of sport over a long period of time causing alterations within the hip. Research has shown a strong, positive correlation between training intensity and radiographic findings of FAI within athletic populations (33,34). It is therefore plausible to suggest that a high intensity of training combined with altered biomechanics can be a causative factor of FAI. This also may account for why FAI occurs in some athletes training at a high level and not others. Again, a great deal of further research into this field is needed to enable definitive conclusions to be drawn.
Conclusion
FAI is an increasing pathology predominantly within the athletic population, but also among the general public. Current research into biomechanical abnormalities in patients with FAI has shown some changes in lower limb and lumbar spine biomechanics when carrying out low intensity tasks. Although this has allowed for some theories to be constructed regarding the effect of FAI on biomechanics, it appears not much research has been conducted in the effects of biomechanics on FAI. Although this article touches on some possible connections between the two, further high-power studies, focusing solely on altered biomechanics as a possible causative factor need to be conducted to allow for changes in thinking in relation to FAI in the future.
Reference List:
1. Leunig M, Beaulé PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clinical orthopaedics and related research. 2009 Mar 1;467(3):616-22.
2. Khusainov NO. Femoroacetabular impingement: literature review. Pediatric Traumatology, Orthopaedics and Reconstructive Surgery. 2015 Jun 15;3(2):42-7.
3. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clinical Orthopaedics and Related Research®. 2003 Dec 1;417:112-20.
4. Hetsroni I, Funk S, Ben-Sira D, Nyska M, Palmanovich E, Ayalon M. Femoroacetabular impingement syndrome is associated with alterations in hindfoot mechanics: A three-dimensional gait analysis study. Clinical Biomechanics. 2015 Dec 1;30(10):1189-93.
5. Zadpoor AA. Etiology of femoroacetabular impingement in athletes: a review of recent findings. Sports Medicine. 2015 Aug 1;45(8):1097-106.
6. Agricola R, Bessems JH, Ginai AZ, Heijboer MP, van der Heijden RA, Verhaar JA, Weinans H, Waarsing JH. The development of Cam-type deformity in adolescent and young male soccer players. The American journal of sports medicine. 2012 May;40(5):1099-106.
7. Lahner M, Walter PA, von Schulze Pellengahr C, Hagen M, von Engelhardt LV, Lukas C. Comparative study of the femoroacetabular impingement (FAI) prevalence in male semiprofessional and amateur soccer players. Archives of orthopaedic and trauma surgery. 2014 Aug 1;134(8):1135-41.
8. Pollard TC, Villar RN, Norton MR, Fern ED, Williams MR, Murray DW, Carr AJ. Genetic influences in the aetiology of femoroacetabular impingement: a sibling study. Bone & Joint Journal. 2010 Feb 1;92(2):209-16.
9. Banerjee P, Mclean CR. Femoroacetabular impingement: a review of diagnosis and management. Current reviews in musculoskeletal medicine. 2011 Mar 1;4(1):23.
10. Cobb J, Logishetty K, Davda K, Iranpour F. Cams and pincer impingement are distinct, not mixed: the acetabular pathomorphology of femoroacetabular impingement. Clinical Orthopaedics and Related Research®. 2010 Aug 1;468(8):2143-51.
11. Hammond CA, Hatfield GL, Gilbart MK, Garland SJ, Hunt MA. Trunk and lower limb biomechanics during stair climbing in people with and without symptomatic femoroacetabular impingement. Clinical biomechanics. 2017 Feb 1;42:108-14.
12. Samaan MA, Schwaiger BJ, Gallo MC, Sada K, Link TM, Zhang AL, Majumdar S, Souza RB. Joint loading in the sagittal plane during gait is associated with hip joint abnormalities in patients with femoroacetabular impingement. The American journal of sports medicine. 2017 Mar;45(4):810-8.
13. Hetsroni I, Funk S, Ben-Sira D, Nyska M, Palmanovich E, Ayalon M. Femoroacetabular impingement syndrome is associated with alterations in hindfoot mechanics: A three-dimensional gait analysis study. Clinical Biomechanics. 2015 Dec 1;30(10):1189-93.
14. Diamond LE, Wrigley TV, Bennell KL, Hinman RS, O’Donnell J, Hodges PW. Hip joint biomechanics during gait in people with and without symptomatic femoroacetabular impingement. Gait & posture. 2016 Jan 1;43:198-203.
15. Crawford JR, Villar RN. Current concepts in the management of femoroacetabular impingement. Bone & Joint Journal. 2005 Nov 1;87(11):1459-62.
16. Leunig M, Beck M, Dora C, Ganz R. Femoroacetabular impingement: etiology and surgical concept. Operative Techniques in Orthopaedics. 2005 Jul 1;15(3):247-55.
17. Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip. Clinical orthopaedics and related research. 2008 Feb 1;466(2):264-72.
18. Brisson N, Lamontagne M, Kennedy MJ, Beaulé PE. The effects of cam femoroacetabular impingement corrective surgery on lower-extremity gait biomechanics. Gait & posture. 2013 Feb 1;37(2):258-63.
19. Shi HY, Mau LW, Chang JK, Wang JW, Chiu HC. Responsiveness of the Harris Hip Score and the SF-36: five years after total hip arthroplasty. Quality of Life Research. 2009 Oct 1;18(8):1053-60.
20. Frank JM, Harris JD, Erickson BJ, Slikker W, Bush-Joseph CA, Salata MJ, Nho SJ. Prevalence of femoroacetabular impingement imaging findings in asymptomatic volunteers: a systematic review. Arthroscopy. 2015 Jun 1;31(6):1199-204.
21. Byrd JT. Femoroacetabular impingement in athletes: current concepts. The American journal of sports medicine. 2014 Mar;42(3):737-51.
22. Philippon MJ, Schenker ML. Arthroscopy for the treatment of femoroacetabular impingement in the athlete. Clinics in sports medicine. 2006 Apr 1;25(2):299-308.
23. Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clinical Orthopaedics and Related Research®. 2006 Apr 1;445:181-5.
24. Leunig M, Slongo T, Ganz R. Subcapital realignment in slipped capital femoral epiphysis: surgical hip dislocation and trimming of the stable trochanter to protect the perfusion of the epiphysis. Instructional course lectures. 2008;57:499-507.
25. Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clinical Orthopaedics and Related Research®. 2004 Dec 1;429:170-7.
26. Byrd JT, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clinical orthopaedics and related research. 2009 Mar 1;467(3):739-46.
27. Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. Bone & Joint Journal. 2001 Nov 1;83(8):1119-24.
28. Sampson TG. Arthroscopic treatment of femoroacetabular impingement. Techniques in Orthopaedics. 2005 Mar 1;20(1):56-62.
29. Heyworth BE, Shindle MK, Voos JE, Rudzki JR, Kelly BT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy. 2007 Dec 1;23(12):1295-302.
30. Kim KC, Hwang DS, Lee CH, Kwon ST. Influence of femoroacetabular impingement on results of hip arthroscopy in patients with early osteoarthritis. Clinical Orthopaedics and Related Research®. 2007 Mar 1;456:128-32.
31. Emara K, Samir W, Motasem EH, Ghafar KA. Conservative treatment for mild femoroacetabular impingement. Journal of Orthopaedic Surgery. 2011 Apr;19(1):41-5.
32. Naal FD, Hatzung G, Müller A, Impellizzeri F, Leunig M. Validation of a self-reported Beighton score to assess hypermobility in patients with femoroacetabular impingement. International orthopaedics. 2014 Nov 1;38(11):2245-50.
33. Lahner M, Walter PA, von Schulze Pellengahr C, Hagen M, von Engelhardt LV, Lukas C. Comparative study of the femoroacetabular impingement (FAI) prevalence in male semiprofessional and amateur soccer players. Archives of orthopaedic and trauma surgery. 2014 Aug 1;134(8):1135-41.
34. Tak I, Weir A, Langhout R, Waarsing JH, Stubbe J, Kerkhoffs G. The relationship between the frequency of football practice during skeletal growth and the presence of a cam deformity in adult elite football players. Br J Sports Med. 2015 May 1;49(9):630-4.